RESEARCH ARTICLE
- Aamir Jalal Al-Mosawi 1
Advisor in Pediatrics and Pediatric Psychiatry, The National Training and Development Center and Baghdad Medical City
*Corresponding Author: Aamir Jalal Al-Mosawi ,Advisor in Pediatrics and Pediatric Psychiatry, The National Training and Development Center and Baghdad Medical City
Citation: Aamir Jalal Al-Mosawi (2024), The novel association of autism with congenital non-syndromic cavum septum pellucidum and its significance: An educational article and expert opinion, Biomedical Studies and Clinical Evaluations (BSCE) 1(1), DOI: https://doi.org/10.64347/3064-7037/BSCE.014
Copyright: © (2024) Aamir Jalal Al-Mosawi this is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 11, 2024 | Accepted: October 15, 2024 | Published: November 10, 2024
Abstract
Background: We have recently described a new therapeutic approach for the treatment of autism disorders which has shown promise in alleviating and curing the major diagnostic features associated with autism. The first book documenting the successful cure of autism patients was recognized in Bookauthority’s lists of best books of all time. Consequently, we have been receiving consultations regarding autism treatment from various regions worldwide. Individualized courses of intramuscular cerebrolysin have emerged as a significant component of the new therapeutic approach contributing to the cure of autism. Autism spectrum disorders have not been reported in association with cavum septum pellucidum.
Patients and methods: This paper describes a boy diagnosed with autism disorder who was found to have cavum septum pellucidum upon brain magnetic resonance imaging (MRI).
Results: Treatment primarily consisted of intramuscular cerebrolysin courses, supplemented with oral risperidone at night, a commonly used neuroleptic for managing hyperactivity. After four months of treatment, the patient exhibited some improvement, estimated at approximately 20% by the father. However, improvement in the two major clinical diagnostic features of autism (response to name and eye contact) was not observed at the clinic. Consequently, brain MRI was performed, revealing the presence of cavum septum pellucidum.
Expert opinion: The current evidence-based expert opinion suggests that the congenital form of isolated large cavum septum pellucidum, presents after two years of age is not an anatomical variation, but a neuro-developmental abnormality that can be asymptomatic, but can predispose to psychiatric disorders including childhood onset schizophrenia. Although autism disorder has been previously reported in association with syndromic cavum septum pellucidum, this paper presents a novel association with non-syndromic cavum septum pellucidum. While this association may be incidental, it could contribute to the less-than-expected response to the new therapeutic approach for autism treatment. Therefore, we recommend performing magnetic resonance imaging in cases of autism with a suboptimal response to treatment. The author hopes that this study contributes to a deeper understanding of the heterogenicity of autism disorders and highlights the importance of comprehensive evaluations of suboptimal response to treatment.
Keywords: Autism, MRI, cavum septum pellucidum, expert opinion
Introduction
We have recently described a new therapeutic approach for the treatment of autism disorders which has shown promise in alleviating and curing the major diagnostic features associated with autism.
The first book documenting the successful cure of autism patients was recognized in Bookauthority’s lists of best books of all time. Consequently, we have been receiving consultations regarding autism treatment from various regions worldwide, including the United Kingdom, Canada, the United Arab Emirates, Tunisia, Palestine, India, and Pakistan, with some international cases being reported.
Individualized courses of intramuscular cerebrolysin have emerged as a significant component of the new therapeutic approach contributing to the cure of autism. Additionally, many patients required neuroleptics such as risperidone, trifluoperazine, and Prochlorperazine to manage hyperactivity and other abnormal behaviors [1-9]. Autism spectrum disorders have not been reported in association with cavum septum pellucidum [10].
The aim of this paper is to report a novel association between autism disorder and magnetic resonance evidence of cavum septum pellucidum and to discuss the significance of this association.
Patients and methods
This paper describes a boy diagnosed with autism disorder who was found to have cavum septum pellucidum upon brain magnetic resonance imaging (MRI).
At approximately three years of age, the boy received a diagnosis of autism disorder. Upon examination, he exhibited two major clinical diagnostic features of autism: lack of response to his name and absence of eye contact. Additionally, he displayed significant hyperactivity and repetitive behaviors.
Treatment primarily consisted of intramuscular cerebrolysin courses, supplemented with oral risperidone at night, a commonly used neuroleptic for managing hyperactivity. After four months of treatment, the patient exhibited some improvement, estimated at approximately 20% by the father. However, improvement in the two major clinical diagnostic features of autism (response to name and eye contact) was not observed at the clinic. Consequently, brain MRI was performed, revealing the presence of cavum septum pellucidum (Figure-1).
Fig -1: Brain magnetic resonance imaging showing cavum septum pellucidum
Discussion
Previous literature has documented various brain imaging abnormalities associated with autism disorders, including agenesis of the corpus callosum, arachnoid cysts, evidence of vasculitis (in Heller syndrome), and brain imaging abnormalities related to coexisting conditions such as cerebral palsy [10]. However, the association between autism disorders and cavum septum pellucidum has not been previously reported.
The septum pellucidum is a thin vertical membrane situated in the midline of the brain, separating the anterior portion of the corpus callosum from the body of the fornix. It divides the anterior horns of the right and left ventricles.
Septum pellucidum was most probably first described by Franciscus de Le Bo Sylvius (Figure-2) in 1671.
Fig-2: Franciscus de Le Bo Sylvius (March 15, 1614-November 19, 1672), a Dutch physician
Septum pellucidum was most probably first described by Franciscus de Le Bo Sylvius (Figure-2) in 1671. Cavum septum pellucidum (Figure-3)
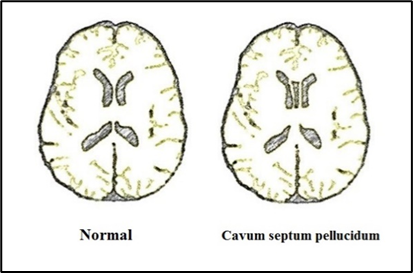
Fig-3: Cavum septum pellucidum is a slit-like cavity in the septum pellucidum
also known as the cave or cavity of the septum pellucidum, is a slit-like cavity between the two leaflets of the septum pellucidum, typically present during fetal development but usually fusing and disappearing during infancy. It was likely first described by Andrea Verga (Figure-4) in 1851, who characterized it as a fluid-filled space.
<!-- /* Font Definitions */ @font-face {font-family:"Cambria Math"; panose-1:2 4 5 3 5 4 6 3 2 4; mso-font-charset:0; mso-generic-font-family:roman; mso-font-pitch:variable; mso-font-signature:-536869121 1107305727 33554432 0 415 0;} /* Style Definitions */ p.MsoNormal, li.MsoNormal, div.MsoNormal {mso-style-unhide:no; mso-style-qformat:yes; mso-style-parent:""; margin:0in; mso-pagination:none; text-autospace:none; font-size:11.0pt; font-family:"Times New Roman",serif; mso-fareast-font-family:"Times New Roman";} .MsoChpDefault {mso-style-type:export-only; mso-default-props:yes; font-family:"Calibri",sans-serif; mso-ascii-font-family:Calibri; mso-ascii-theme-font:minor-latin; mso-fareast-font-family:Calibri; mso-fareast-theme-font:minor-latin; mso-hansi-font-family:Calibri; mso-hansi-theme-font:minor-latin; mso-bidi-font-family:"Cordia New"; mso-bidi-theme-font:minor-bidi;} .MsoPapDefault {mso-style-type:export-only; margin-bottom:8.0pt; line-height:107%;} @page WordSection1 {size:8.5in 11.0in; margin:1.0in 1.0in 1.0in 1.0in; mso-header-margin:.5in; mso-footer-margin:.5in; mso-paper-source:0;} div.WordSection1 {page:WordSection1;} -->
Fig-4: Andrea Verga (1811-1895), an Italian physician
Several pathologies of cavum septum pellucidum have been reported in the medical literature during the 1950s and early 1960s, including dilation (Fattovich, 1954), abscess (Hughes and colleagues, 1955), pseudocyst (Vullo, 1957), cysts (Aparicio lopez and Escalona Zapata, 1959), and hemorrhage (Gerlach and Kautzky) [11-16].
In 1981, Farruggia and Babcock reported that brain ultrasound study of 102 infants showed that cavum septum pellucidum was present in 42% of the studied infants, and in 61% of the studied premature infants, and in 50% of the studied full-term infants. The largest cavum septum pellucidum was 10 mm in width [17].
In 1983, Akiyama et al reported that seventy-one patients of 2722 who had a brain CT-scanning were found to have cavum septum pellucidum. 2.6% of the 71 patients had visited a mental clinic. Epileptic attacks were found in 22.5% of the patients, and mental retardation was found in 9.9% of the 71 patients [18].
In 1990, Bodensteiner and Schaefer from the United States reported that a wide cavum septum pellucidum (More than 10 mm of the leaves) may be associated with cognitive impairment and seizures, and may indicate an abnormal development [19].
In 1992, Degreef et al emphasized that cavum septum pellucidum is a developmental anomaly that was found on magnetic resonance imaging in 17 of 81 patients (21%) who had schizophrenia compared to only one individual (2%) of 46 control individuals. Cavum septum pellucidum was also found in post-mortem study of 17 of 28 (61%) patients with schizophrenic compared with 12 of 39 (31%) normal controls [20].
In 1996, in 1996, Shioiri et al. from Japan found that patients with schizophrenia exhibited a higher incidence of moderate to large cavum septum pellucidum compared to control individuals.
They emphasized that cavum septum pellucidum is a developmental anomaly that generally associated with no clinical manifestations. They studied the magnetic resonance imaging findings of 113 patients who had affective disorders (69 patients with bipolar disorder and 44 patients with major depression), 40 patients who had schizophrenia, and 92 control individuals. They found that patients with schizophrenia had considerably higher incidence of moderate to large cavum septum pellucidum compared with the control individuals.
The finding of Shioiri et al suggested that cavum septum pellucidum is a neuro-developmental abnormality that can predispose the individual to the development of schizophrenia [21].
In 1998, Nopoulos et al. from the United States observed enlarged cavum septum pellucidum in a subset of children with childhood-onset schizophrenia. They reported the magnetic resonance imaging findings of 24 patients (Mean age: 14.6 years).who had childhood-onset schizophrenia. Three of the 24 (12.5%) children had enlarged cavum septum pellucidum, while only one of 95 control individuals (1.1%) had cavum septum pellucidum [22].
Also in 1998, Guru Raj et al from Malaysia reported that 54 of 1281 patients who had a brain CT-scanning were found to have cavum septum pellucidum. Recurrent seizures and developmental delay were the most common associated clinical manifestation. 75.9% of the patients had marked neurological deficits. 76% of the patients had other cerebral abnormalities including cortical atrophy, cerebral infarction and hydrocephalus [23].
In 2019, Wang et al. from China conducted a review indicating a higher prevalence of cavum septum pellucidum in patients with mental disorders compared to healthy controls. They reviewed 25 controlled studies which included 2392 patients who had mental disorders and 1445 healthy controls. They found that cavum septum pellucidum was present in much more patients with mental disorders than in healthy individuals [24].
In 2024, Zhang et al from China reported a case of Chinese boy aged 21 months who had a syndromic form of cavum septum pellucidum associated autism disorder and other neuro-developmental abnormalities including severe generalized developmental delay, seizures, craniofacial deformity, hypotonia, and corpus callosum malformation [25].
This paper presents a boy who was treated with a recently introduced therapeutic approach for the treatment of autism and reports a previously unexplored association between autism disorders and cavum septum pellucidum. This paper contributes to the growing body of knowledge on autism disorder etiology and treatment strategies, highlighting the importance of considering developmental brain anomalies in therapeutic interventions.
Expert opinion
The current evidence-based expert opinion suggests that the
congenital form of isolated large cavum septum pellucidum, presents after two years of age is not an anatomical variation, but a neuro-developmental abnormality that can be asymptomatic, but can predispose to psychiatric disorders including childhood onset schizophrenia.
Although autism disorder has been previously reported in association with syndromic cavum septum pellucidum, this paper presents a novel association with non-syndromic cavum septum pellucidum. While this association may be incidental, it could contribute to the less-than-expected response to the new therapeutic approach for autism treatment. Therefore, we recommend performing magnetic resonance imaging in cases of autism with a suboptimal response to treatment.
The author hopes that this study contributes to a deeper understanding of the heterogenicity of autism disorders and highlights the importance of comprehensive evaluations of suboptimal response to treatment
Acknowledgement
The author has the copyright of all the sketches and figures included in this paper.
Conflict of interest: None
References
-
Al-Mosawi AJ. Cure of Autistic Disorders: Mission Impossible is Possible in an Illustrated Pioneering Experience. SunKrist Journal of Psychiatry and Mental Health 2020 August 21; 1 (1):1-20. Doi: 10.5281/ zenodo.4014755.
Publisher | Google Scholor -
Al-Mosawi AJ. Books of Aamir Jalal Al-Mosawi included in Bookauthority’s list of Best Books of All Time on December 15, 2021. Doi: 10.13140/RG.2.2.12396.90240.
--> -
Al-Mosawi AJ. Best Iraqi medical books of all time: History of medicine. LAP LAMBERT Academic Publishing: 2023 (ISBN: 978-620-6-75283-7).
Publisher | Google Scholor -
Al-Mosawi AJ. I migliori libri di medicina iracheni di tutti i tempi: Storia della medicina (Italian edition). Edizioni Sapienza: 2023 (ISBN: 978-620-6-40368-5).
--> -
Al-Mosawi AJ. Cerebral Palsy and Autism Associated With Periventricular White Matter Hyperintensity on Brain Magnetic Resonance Imaging: A New Disorder and Its Treatment. MedPress Psychiatry and Behavioral Sciences 2022; 1(1):1-4 [mppbs–202209007]. Doi: 10.5281/zenodo.7181688.
Publisher | Google Scholor -
Al-Mosawi AJ. Treatment of Williams syndrome: Evidence-based medicine and expert opinion .Biomedical and Biotechnological Sciences July 21 2022; 1(2): 1-3. Doi: 19.0810/BBS.2022/0006.
Publisher | Google Scholor -
Al-Mosawi AJ. Treatment of a girl from Tunisia with typical autism: Evidence-based medicine and expert opinion. Biomedical and Biotechnological Sciences Aug 2022; 1(2): 1-5. Doi: 10.0810/BBS.2022/0008.
Publisher | Google Scholor -
Al-Mosawi AJ.A girl from Pakistan with atypical autism: Expert opinion and a therapeutic recommendation. World Journal of Radiology and Imaging 07 Nov 2022; 1(1): 38-41.Doi: 10.5281/zenodo.7371723.
Publisher | Google Scholor -
Al-Mosawi AJ. A Case of Atypical Autism with Mental Retardation in an Adult from Canada: An Educational Article and Expert Opinion. Journal of Brain and Neurological Disorders (ISSN: 2642-973X) 17 June 2023; 6(4): 1-5. Doi: 10.31579/2642-973X/058.
Publisher | Google Scholor -
Al-Mosawi AJ. Brain Imaging Abnormalities in Autism Disorders. Journal of Clinical Research in Radiology (ISSN: 2639-913X) 2020; 3 (2): 1-3.
Publisher | Google Scholor -
Pearce JM. Some observations on the septum pellucidum. Eur Neurol 2008;59(6):332-4. Doi: 10.1159/000121428.
Publisher | Google Scholor -
Fattovich G. Considerazioni su alcuni casi dilatazione del cavo del setto pellucido [Study of several cases of dilation of the cavum septi pellucidi]. Rass Studi Psichiatr 1954; 43(4):653-72 [Article in Italian].
--> -
Hughes RA, Kernohan JW, Woltman HW. Abscess of cavum septum pellucidum: report of a case. Proc Staff Meet Mayo Clin 1955 Nov 16; 30(23):536-8.
Publisher | Google Scholor -
Vullo C. Su di un caso di pseduo-cisti del cavo del setto pellucido [Case of pseudocyst of cavum septi pellucidi]. Arcisp S Anna Ferrara. 1957; 10(4):829-37 [Article in Italian].
Publisher | Google Scholor -
Aparicio lopez O, Escalona Zapata J. [Cysts of the septum pellucidum and of the cavum vergae]. Rev Clin Esp. 1959 May 31; 73:246-54 [Article in Spanish].
Publisher | Google Scholor -
Gerlach J, Kautzky R. [Hemorrhage from an aneurysm into a cavum septi pellucidi]. Zentralbl Neurochir. 1960; 20:127-34 [Article in German].
Publisher | Google Scholor -
Farruggia S, Babcock DS. The cavum septi pellucidi: its appearance and incidence with cranial ultrasonography in infancy. Radiology 1981 Apr; 139(1):147-50.Doi: 10.1148/ radiology.139.1.7208915.
Publisher | Google Scholor -
Akiyama K, Sato M, Sora I, Otsuki S, Wake A, Fukui H, Takahashi Y, Yanagida K, Sudara M. [A study of incidence and symptoms in 71 patients with cavum septi pellucidi]. No To Shinkei 1983 Jun; 35(6):575-81 [Article in Japanese].
Publisher | Google Scholor -
Bodensteiner JB, Schaefer GB. Wide cavum septum pellucidum: a marker of disturbed brain development. Pediatr Neurol 1990 Nov-Dec; 6(6):391-4. Doi: 10.1016/ 0887-8994(90)90007-n.
Publisher | Google Scholor -
Degreef G, Bogerts B, Falkai P, Greve B, Lantos G, Ashtari M, Lieberman J. Increased prevalence of the cavum septum pellucidum in magnetic resonance scans and post-mortem brains of schizophrenic patients. Psychiatry Res. 1992 May; 45(1):1-13. Doi: 10.1016/0925-4927(92)90009-s.
Publisher | Google Scholor -
Shioiri T, Oshitani Y, Kato T, Murashita J, Hamakawa H, Inubushi T, Nagata T, Takahashi S. Prevalence of cavum septum pellucidum detected by MRI in patients with bipolar disorder, major depression and schizophrenia. Psychol Med 1996 Mar; 26(2):431-4. Doi: 10.1017/s0033291700034838.
Publisher | Google Scholor -
Nopoulos PC, Giedd JN, Andreasen NC, Rapoport JL. Frequency and severity of enlarged cavum septi pellucidi in childhood-onset schizophrenia. Am J Psychiatry 1998 Aug; 155(8):1074-9. Doi: 10.1176/ajp.155.8.1074.
Publisher | Google Scholor -
Guru Raj AK, Pratap RC, Jayakumar R, Ariffin WA. Clinical features and associated radiological abnormalities in 54 patients with cavum septi pellucidi. Med J Malaysia 1998 Sep; 53(3):251-6.
Publisher | Google Scholor -
Wang LX, Li P, He H, Guo F, Tian P, Li C, Cui LB, Xi YB, Yin H. The Prevalence of Cavum Septum Pellucidum in Mental Disorders Revealed by MRI: A Meta-Analysis. J Neuropsychiatry Clin Neurosci 2020 Spring; 32(2):175-184. Doi: 10.1176/appi. Neuro psych.18030060.
Publisher | Google Scholor -
Zhang X, Han Y, Yang L, Xu N, Zhu L, Qiu S, Li Y, Xu L, Yu X. Clinical phenotype and genetic characteristics of SZT2 related diseases: A case report and literature review. Seizure 2024 Jan; 114:111-120. Doi: 10.1016/j.seizure.2023.12.008.
Publisher | Google Scholor
